From birth, in fact even during the birth process, humans become colonised by microbes. They live on our skin, in our hair and in our guts, and there is growing evidence that they influence every facet of our lives from our diet to our mental health (1). Quite simply, microbes can alter the way we experience being human.
We’re complex organisms. Moving a muscle, digesting our breakfast, solving problems and communicating with others all involve interactions between neural and muscular pathways. Scientists have discovered that all types of bacteria – commensal (neutral), probiotic (beneficial) and pathogenic (harmful) – can activate neural pathways and the Central Nervous System (CNS), which sends messages to and from the brain (2).
This has led to the coining of the phrase, the “gut-brain axis” (1). It refers to the reciprocal communication between the organisms living in your gut and your brain. These microbes act on the brain and the brain acts on the gut.
The figure below illustrates the extent of this bilateral communication and the impacts that this can have on our health.
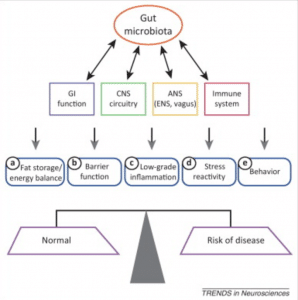
Figure 1. Communication between the gut and other body systems can influence the balance between health and disease. Image credit: Foster & McVey Neufeld. Trends in Neurosciences. 2013
- GI: Gastrointestinal tract (esophagus, stomach, large and small intestines)
- CNS: Central nervous system; neural communication between the brain and spinal cord
- ANS: Autonomic nervous system; it works largely unconsciously and controls functions such as heart rate and urination.
- Immune system: responds to infection, involved in allergic reactions and hypersensitivities
So why does this matter?
The composition of the human gut is as unique as our fingerprints. However, recent studies have suggested that there are two key aspects of the gut microbiome which are important for overall health: general composition and stability (3). Although individual microbiomes may vary widely, there are some bacteria which are associated with better health and wellbeing. These include lactobacilli and other ‘good’ bacteria that produce helpful compounds, such as essential amino acids. Perhaps more important though is the stability of your microbiome. Scientists have discovered that fluctuations in the composition and diversity of your microbiome can increase inflammation, alter your immune response and increase stress (1,3). This is because of the way bacteria can alter signalling within the CNS.
Your microbiome composition can be altered very early in life through factors such as breast-feeding, birth by Caesarean section, stress or infection. In combination with your genetics, these factors produce your microbiome. Your microbiome can then be altered throughout your life through environmental factors such as diet and medications. Despite this, your initial microbiome can still have long-term impact on how you respond to stress (4). Therefore, the key question is whether your microbiome can be modified to such an extent that it may have therapeutic benefits for stress-related disorders. There is evidence to suggest that your diet can alter not only which bacteria are present in your gut, but how many there are, and how they interact with your immune and nervous systems (4).
Broadly, the presence of probiotic bacteria has been shown to reduce anxiety-like behaviours in male mice, when they were subjected to maze, open field and forced swimming tests (1). In particular, a lack of bacteria, perhaps as a result of chronic exposure to broad-spectrum* antibiotics, impacts multiple stress pathways across multiple organ systems and areas of the brain. This suggests that increasing probiotics in your diet, especially after antibiotic treatment, can help you to maintain a healthy gut flora and decrease anxious behaviour during times of stress (1,3).
So while this is all very interesting, what does it mean? How can you use this information?
It’s important to note that almost all of the studies undertaken to date have been with mice. Mice are great animal models, sharing many physiological characteristics with humans. Nevertheless, there are important differences, which is why we conduct human clinical trials before licensing medications or other therapeutic options. Microbiome studies in humans have been correlative, not experimental. This means that researchers have analysed the gut microbiomes of people and compared them with their health/medical profile, in order to make inferences about the influence of the microbiome on our overall health. This is an emerging (and incredibly exciting) area of science, with the potential to transform how we treat health and disease in humans.
For now, aim to eat a varied diet based on whole foods. This is especially important if you’re older, as the stability of your microbiome can decrease with age, meaning any changes in diet can result in a more significant fluctuation in the composition of your gut flora. Consider eating foods high in ‘good’ bacteria, including yoghurt and fermented products such as sauerkraut. If you need to be on antibiotics, chat to your GP about taking probiotics once the course is finished. And watch this space, because you’ll be hearing a lot more about your gut in the next few years than you ever thought possible!
*Broad-spectrum antibiotics target a wide-range of bacterial species, meaning that they will kill not only pathogenic bacteria (which cause an infection), but commensal and probiotic bacteria too.
Reference List
- Foster, J & McVey Neufeld, KA 2013, Gut-brain axis: how the microbiome influences anxiety and depression’, Trends in Neurosciences, vol. 36, no. 5, pp.305-312.
- Lyte, M 2013, ‘Microbial Endocrinology in the Microbiome-Gut-Brain Axis: How Bacterial Production and Utilization of Neurochemicals Influence Behaviour’, PLoS Pathogens, vol. 9, no.11, pp.e1003726.
- Cryan, JF & O’Mahony SM 2011, ‘The microbiome-gut-brain axis: from bowel to behaviour’, Neurogastroenterology & Motility, vol. 23, no.3, pp.187-192.
- Foster, J, Rinaman L & Cryan, J 2017, ‘Stress and the gut-brain axis: Regulation by the microbiome’, Neurobiology of Stress, vol. 7, pp. 124-136.
About the Author – Rachael Dodds
Rachael has been a Studio Pilates client since 2002 and started working at Studio Pilates HQ in 2013. She is passionate about the transformative impact these classes have had on her physical and mental wellbeing. She recently graduated with a Bachelor of Science (Microbiology) and Bachelor of Arts (Anthropology) from the University of Queensland. She was an elite track athlete for 9 years, representing Australia at the Athletics World Championships in 2011 and London 2012 Paralympic Games.