Article categories, Injuries and Pregnancy
A Pilates Instructor’s Guide to Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disorder which affects the nervous system and the body’s movement. It is the second most common neurodegenerative disease in the world behind Alzheimer’s disease (“Neurodegenerative Diseases”, 2022).

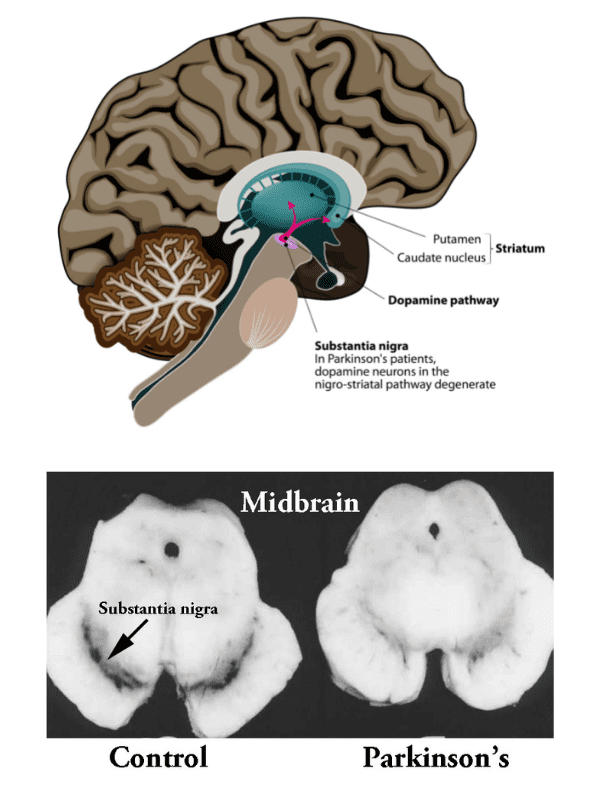
The development of Parkinson’s disease is linked to an area of the brain called the substantia nigra.
The substantia nigra is located in the “midbrain” and is comprised of pigmented cells which appear dark in appearance due to a high neuromelanin content. The Latin words “substantia nigra” translate to “black substance,” which describes the appearance of this part of the brain. The substantia nigra is critical in the production of dopamine and plays a large role in movement and coordination of the body.
Parkinson’s disease develops when the dopamine neurons (nerve cells) in the substantia nigra are damaged and die over time. On an MRI of a healthy brain, it is possible to see the black area of the substantia nigra, however on a patient with Parkinson’s disease, this dark area is less noticeable, indicating damage, degeneration or death to the neurons in this area of the brain.

Parkinson’s is a progressive disease, with symptoms appearing gradually and becoming more severe over time.
The most common symptoms include motor problems such as –
- Tremors in the hands, arms, legs, jaw or head
- Stiff/rigid limbs
- Slow movement (called Bradykinesia)
- Difficulty with balance, gait and coordination

The cause of Parkinson’s disease is not fully understood, but research suggests that genetics, environmental exposures (exposure to heavy metals, pesticides etc.) and a past history of head trauma may contribute to the disease’s development. While the disease can affect both men and women, research suggests that it is more common in men and most commonly occurs in patients aged over 60, although it can also be less commonly present in younger patients (“Parkinson’s Disease Risk Factors and Causes”, 2022).

While there is currently no cure for Parkinson’s disease, treatment may involve –
- Physical therapy and exercise
- Medication to increase dopamine levels
- Surgery (such as deep brain stimulation)
- Speech and occupational therapy
- Complementary therapies such as massage and acupuncture

Postural and gait changes are commonly experienced in people with Parkinson’s disease due to stiff muscles or periods of time off medication. Postural changes may include –
- Exaggerated kyphosis in the upper spine
- Protracted neck (forward head posture)
- Protracted/rounded shoulders
- A stooped posture
- Leaning sideways/lateral flexion through the spine
- Shuffling gait

Exercise can be incredibly beneficial for anyone with Parkinson’s disease and research suggests that it can reduce symptoms and improve quality of life (“Exercise”, 2022). The Parkinson’s Foundation recommends the following exercise guidelines for people with Parkinson’s disease –
- Performing 150 minutes of moderate to vigorous exercise per week
- Modifying and progressing the exercise routine over time
- Incorporating aerobic activity, strength training, balance/agility/multitasking and stretching
The Parkinson’s Foundation also recommends that the following safety considerations are taken into account with any fitness program –
- Supervision is important in the event of low blood pressure or “freezing of gait”
- Be aware that full range of motion may not be possible due to muscle stiffness, adapt accordingly
- Ensure safety with balance-based exercises and encourage the client to hold onto something stable to assist with balance and prevent falls

Some studies suggest that the benefits of Pilates “on lower-body function appear to be superior to those of other conventional exercises” for people with Parkinson’s disease (Suárez-Iglesias et al., 2019).
Pilates may also benefit people with Parkinson’s disease through improving –
- Flexibility
- Balance and coordination
- Mind to muscle connection
- Overall fitness
- Reducing pain
- Providing greater mobility

- People with Parkinson’s often have trouble initiating the movement (this is often referred to as “freezing”), so whatever exercise you get them to perform, they may need more assistance and physical guidance with cueing and demonstrations to get them started with the movement. Then once they have the movement, keep them going with that movement until fatigue sets in (you want to avoid constantly swapping and changing the exercise after a few reps)
- Following the Studio Pilates Cueing Formula will be incredibly beneficial for clients with Parkinson’s disease as this formula provides a sequential way to perform and understand the movement (from getting into the correct position first, to beginning the exercise, to finishing the exercise safely)
- Depending on the severity of the Parkinson’s disease, the client may have visible tremors or shaking of the limbs/body when performing exercise. This is involuntary and is not a contraindication to performing the exercise (assuming that the client is comfortable and pain free)
- Pilates with the studio equipment (Reformer, Cadillac etc.) may be more suitable so the client doesn’t need to get up and down off the ground (Matwork Pilates may pose some challenges with getting up and down off the mat)
- If the client is experiencing pain, only work within their limits and this includes possibly decreasing the range of movement
- Be aware that the client may have low blood pressure and may feel dizzy or lightheaded when moving from sitting or lying to standing
- The client may fatigue, so adjust session times based on when it is best for the client and end classes earlier when needed
- Some clients may have greater energy at different times of the day so plan sessions around this (ie. many people with Parkinson’s disease report fatigue later in the day. If this is the case, plan a morning session)
- Be aware that balance will likely be affected and ensure that the client is safe the whole time – get the client to hold onto a stable surface to assist with balance

People with Parkinson’s disease are likely to be –
- Tight and stiff through the thoracic spine, especially if they have a stooped posture which is creating flexion through the thoracic spine (exaggerated kyphosis) – gentle thoracic extension and rotation stretches can help with this
- Tight through the Psoas and hip muscles – focusing on gentle hip mobility can help with this
- Tight through the Latissimus Dorsi
- Tight through the Pecs and chest due to rounded and protracted shoulders
- Generally weak through all muscles

General
- Ideally perform matwork exercises on an elevated surface such as on a Reformer or Cadillac (so the client does not need to get up and down off the floor)
- If you need to perform matwork on the floor, be very aware of your programming so that the client does not need to get up and down off the floor constantly – minimise position changes as much as possible
Supine Abdominal Series
- If the client has a stooped posture, keep the head down (the repeated head lifting may not be comfortable for anyone with a stooped posture)
- Use a head cushion if comfortable
- Start with lower level abdominals with the feet down (Bent Knee Fallouts, Lift Foot, Leg Slides etc)
- Then gradually progress to Tabletop position (with exercises like Toe Taps and Pendulum – use smaller range of movement)
- Depending on the progression of disease, the client may or may not be able to move onto leg extension exercises (Like Bicycle Legs and Criss Cross)
Supine Buttock Series
- A great series for anyone with Parkinson’s disease as there is extremely low risk of falls
- All exercises should be safe to perform except for Pelvic Curl 3 (Single Leg Lift)
- Instead you can add more levels and modifications to the Pelvic Curl exercises through adding in resistance bands or small balls between the knees
- It may be more ideal to perform the Pelvic Curl exercises with a straight back/neutral spine instead of rolling through the spine (this is because if the client’s posture is stooped or leaning to the side / laterally flexed, the client may have reduced range of movement through the spine)
Side Lying Series
- A relatively safe series for people with Parkinson’s disease
- However if a pronounced lateral flexion is present, the client may not be able to lie down comfortably on one side. If this is the case, avoid this series
- Clam exercises are a great option if the client is able to lie on their side
- Progressive Gluteal exercises like Hot Potato, Rectangles and Bicycles can be performed but require more coordination and balance
- Double Leg Lift exercise can be performed, however be aware that these may be challenging for balance. If the client is laterally flexed, they may be more likely to feel this in their back muscles. Keep the head down.
Prone Lying Series
- Mid and upper back exercise are usually a good option for people with Parkinson’s disease, however performing exercises in prone may be uncomfortable for someone with a stooped posture
- Instead modify these exercises to perform in kneeling or standing (standing may be more suitable for older clients)
Kneeling Series
- Four point kneeling exercises may be beneficial depending on the severity of Parkinson’s disease as this position is quite stable and provides more global strengthening of the body
- If the client is able to four point kneel, the Horsekick exercises are a great option. Avoid Horsekick 3 (Sidekick) as this requires greater balance and range of movement
- Avoid Kneeling Sidekick and Hinge exercises as these may put too much pressure on the joints and require more advanced balance
Plank Series
- Perform Plank on the knees
- Modify Pilates Push Ups to be performed against a wall or on an elevated surface like a kitchen bench (to make the exercise easier and avoid pressure on the joints)
- Avoid Tricep Circles
Stretching Series
- Exercise caution with Spiral Stretch and Mermaid Stretch as the client may have difficulty getting into these positions and performing the stretch safely
- Avoid Gluteal Stretch Prone and Rolldown Stretch
- All other stretches in the Matwork Course should be safe to perform

General
- Depending on the severity of Parkinson’s disease, only place clients in positions where they can be safe and stable without risk of falling
- Keep movements and exercises simple
- The spring resistance can be incredibly beneficial for clients with Parkinson’s disease and resistance training is recommended by the Parkinson’s Foundation
Supine Abdominal Series
- If the client has a stooped posture, keep the head down (the repeated head lifting may not be comfortable for anyone with a stooped posture)
- Use a head cushion if comfortable
- Start with lower level abdominals. If clients can’t perform tabletop position, stick to the Matwork exercises with the feet down (Bent Knee Fallouts, Lift Foot etc). These can be performed lying on the reformer with the feet on the standing platform
- Then gradually progress to Tabletop position (with exercises like Abdominal Curl)
- Depending on the progression of disease, the client may or may not be able to move onto leg extension exercises (Like Bicycle Legs and Criss Cross)
Midback Series
- All exercises should be safe to perform
- The safest arm series for people with Parkinson’s to perform
Back Rowing Series
- Clients may sit on the box or sit cross legged on the carriage. However sitting cross legged on the carriage may pose difficulties for clients with poor flexibility
- Ensure that you spot the client sitting on the box to prevent falls
- Most clients with early stage Parkinson’s disease will be able to perform all of these exercises
- A great series to perform as it is the second safest arm series to perform for people with Parkinson’s disease and will help to improve upper back posture
Front Rowing Series
- The Front Rowing Series requires more balance and stability so only get clients to perform this series if they are capable of doing so safely
- Do not perform this series kneeling due to balance risk, instead perform this series sitting on a box and spot the client the whole time
Side Arm Series
- Clients may sit on the box or sit cross legged on the carriage. However sitting cross legged on the carriage may pose difficulties for clients with poor flexibility
- Ensure that you spot the client sitting on the box or sitting on the carriage to prevent falls
- Most clients with early stage Parkinson’s disease will be able to perform all of these exercises
- Be sure to spot the client the whole time for safety
- Do not perform this series kneeling due to balance risk, instead perform this series sitting on a box and spot the client the whole time
- People with Parkinson’s disease often develop shoulder problems such as Frozen Shoulder. As such, exercises like Internal Rotation and External Rotation which strengthen the Rotator Cuff muscles can be really beneficial for these clients
- Stick with the easier exercises in the series, may need to avoid more complicated larger movements like Draw a Sword
Prone Arm Series
- A good series to perform in the early stages of Parkinson’s disease or for any clients who don’t have a pronounced kyphosis or stooped posture – good for helping to prevent pronounced kyphosis developing or a stooped posture from developing
- However for anyone who already has a pronounced kyphosis or stooped posture, they may find that this series strains their neck
- If performing, assist the client to get on and off the box safely
Footwork Series
- Most clients will be able to perform the Footwork Series safely
- The exercises Running, Single Leg Stretch 2 (Bicycles), Pelvic Curl 3 (Single Leg Lift) and Hamstring Curls may require more coordination and may be too challenging
- It may be more ideal to perform the Pelvic Curl exercises with a straight back/neutral spine instead of rolling through the spine (this is because if the client’s posture is stooped or leaning to the side / laterally flexed, the client may have reduced range of movement through the spine and this can feel uncomfortable)
- For the Footwork exercises (either single leg or double leg), if a client’s legs are shaking due to tremors and if this causes the feet to move on the footbar, you may need to hold the client’s ankles and secure the feet on the footbar so they do not slip off
Feet in Straps Series
- This series may be okay to perform for clients in the early stages of Parkinson’s disease
- However in later stages of the disease, the tremors/shaking making these exercises challenging to perform. It also may be difficult to get the feet in the straps. Some exercises like Big Frog also involve more complicated movements
Side Lying Series
- Avoid Foot in Strap exercises as these will be harder to coordinate with tremors/shaking
- Foot on Bar exercises should be safe to perform
- For the Foot on Bar series, if a client’s leg is shaking due to tremors and if this causes the foot to move on the footbar, you may need to hold the client’s ankle and secure the foot on the footbar so it does not slip off
- Double Leg Lift exercises should be safe to perform in the early stages of Parkinson’s but may be challenging for balance in the later stages. Keep the head down. Beats and Scissors modifications may be harder to coordinate.
Kneeling Series
- Knee Stretches 1 (Knees Down) and Reverse Knee Stretches should be safe to perform with guidance
- Avoid Hinge due to balance and pressure on joints
- Avoid Knee Stretches 2 (Knees Off) and Knee Stretches 3 (Running Preparation)
Short Box Series
- Avoid this series due to balance concerns
Plank Abdominal Series
- Avoid this series
- Perform Plank on the Mat on the knees instead
- Modify Push Ups to be performed against a wall or on an elevated surface like a kitchen bench (to make the exercise easier and avoid pressure on the joints)
Standing Series
- Avoid all exercises standing on the reformer due to balance/safety concerns
- Okay to perform Scooter but get the client to hold onto the footbar for safety and balance
Stretching Series
- Exercises safe to perform: Lat Stretch, Calf Stretch, Hip Flexor Stretch 1 (Hands on Footbar)
- Spider Stretch 1 (Foot on the Floor) may be safe to perform in the early stages
- Modify Kneeling Quad Stretch to be standing next to the reformer facing the pulleys. Place the foot of the leg closest to the reformer on the footbar and the knee of the same leg on the carriage.
- Avoid Front Split Stretch, Glute Stretch on the Footbar, Mermaid Stretch,
- Inner Thigh Feet in Straps Stretch and Hamstring Foot in Strap Stretch may be possible in the early stages to perform depending on severity of disease, flexibility, amount of temor, and ability to put the feet in the straps

Bae, Y., Kim, J., Sohn, C., Choi, J., Choi, B., & Song, Y. et al. (2021). Imaging the Substantia Nigra in Parkinson Disease and Other Parkinsonian Syndromes. Radiology, 300(2), 260-278. https://doi.org/10.1148/radiol.2021203341
Bakhshayesh, B., Sayyar, S., & Daneshmandi, H. (2017). Pilates Exercise and Functional Balance in Parkinson’s Disease. Caspian Journal Of Neurological Sciences, 3(8), 25-38. https://doi.org/10.18869/acadpub.cjns.3.8.25
Bradykinesia. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Movement-Symptoms/Bradykinesia-Slowness-of-Movement.
Cancela, J., Mollinedo Cardalda, I., Ayán, C., & de Oliveira, I. (2018). Feasibility and Efficacy of Mat Pilates on People with Mild-to-Moderate Parkinson’s Disease: A Preliminary Study. Rejuvenation Research, 21(2), 109-116. https://doi.org/10.1089/rej.2017.1969
Damier, P., Hirsch, E., Agid, Y., & Graybiel, A. (1999). The substantia nigra of the human brain. Brain, 122(8), 1437-1448. https://doi.org/10.1093/brain/122.8.1437
Exercise. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Treatment/Exercise.
J, S., V, R., & MR, B. (2022). Neuroanatomy, Substantia Nigra. PubMed. Retrieved 13 April 2022, from https://pubmed.ncbi.nlm.nih.gov/30725680/.
Johnson, L., Putrino, D., James, I., Rodrigues, J., Stell, R., Thickbroom, G., & Mastaglia, F. (2022). The effects of a supervised Pilates training program on balance in Parkinson’s disease. Retrieved 13 April 2022, from https://www.scirp.org/Journal/PaperInformation.aspx?PaperID=31424.
Khlebtovsky, A., Djaldetti, R., Rodity, Y., Keret, O., Tsvetov, G., Slutzcki-Shraga, I., & Benninger, F. (2017). Progression of postural changes in Parkinson’s disease: quantitative assessment. Journal Of Neurology, 264(4), 675-683. https://doi.org/10.1007/s00415-017-8402-6
Neurodegenerative Diseases. National Institute of Environmental Health Sciences. (2022). Retrieved 13 April 2022, from https://www.niehs.nih.gov/research/supported/health/neurodegenerative/.
Pantall, A., Suresparan, P., Kapa, L., Morris, R., Yarnall, A., Del Din, S., & Rochester, L. (2018). Postural Dynamics Are Associated With Cognitive Decline in Parkinson’s Disease. Frontiers In Neurology, 9. https://doi.org/10.3389/fneur.2018.01044
Parkinson’s Disease. nhs.uk. (2022). Retrieved 13 April 2022, from https://www.nhs.uk/conditions/parkinsons-disease/.
Parkinson’s Disease – Symptoms and Causes. Mayo Clinic. (2022). Retrieved 13 April 2022, from https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055.
Parkinson’s Disease Risk Factors and Causes. Hopkinsmedicine.org. (2022). Retrieved 13 April 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/parkinsons-disease/parkinsons-disease-risk-factors-and-causes.
Parkinson’s Exercise Recommendations. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/pd-library/fact-sheets/Parkinsons-Exercise-Recommendations.
Physical Therapy. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Treatment/Physical-Therapy.
Suárez-Iglesias, D., Miller, K., Seijo-Martínez, M., & Ayán, C. (2019). Benefits of Pilates in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Medicina, 55(8), 476. https://doi.org/10.3390/medicina55080476
Stooped Posture. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Movement-Symptoms/Stooped-Posture.
Surgical Treatment Options. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Treatment/Surgical-Treatment-Options.
Treatment. Parkinson’s Foundation. (2022). Retrieved 13 April 2022, from https://www.parkinson.org/Understanding-Parkinsons/Treatment.
Triarhou, L. (2022). Dopamine and Parkinson’s Disease. Ncbi.nlm.nih.gov. Retrieved 13 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK6271.
Xing, Y., Sapuan, A., Dineen, R., & Auer, D. (2018). Life span pigmentation changes of the substantia nigra detected by neuromelanin-sensitive MRI. Movement Disorders, 33(11), 1792-1799. https://doi.org/10.1002/mds.27502

